Introduction to Legionella and Legionnaires' disease in Europe
From 2011 to 2015, 30,532 cases of Legionnaires' disease (LD) were reported to the European Centre for Disease Prevention and Control (ECDC).
The annual number of reported cases of Legionnaires' disease increased by 42% between 2011 and 2015.4 The overall notification rate was 1.37 per 100,000 of the population, which was the highest ever observed, and the mortality rate was 8.1%.5Several factors have contributed to the increase of Legionnaires' cases in Europe. Previous studies have suggested that changing environmental conditions, especially in rainfall and temperature, have affected the number of cases 6 7 8. Additionally, the population structure of the EU/EEA is changing, with an increasing proportion of older persons who are more at risk of infection.
Nevertheless, with effective water management, Legionnaires' disease is completely preventable. ECDC has published guidelines that should be used to manage the risk of contracting Legionella, thereby protecting public health.
Guidelines for the prevention and control of Legionella in Europe
Since the publication of the WHO’s Water Safety in Buildings in 2011, The Water Safety Plan (WSP) approach is being adopted across European countries as the most effective way to minimise risks from poor water quality from source to point of use. It is a preventive approach which aims to identify weak points in a system where waterborne hazards could enter, and which might increase within the system to levels which pose a risk to users and anyone else who may be exposed.
This approach includes all water systems such as cooling towers, water tanks, pools, spa, fountains, misters, showers and others. Furthermore, the WSP encourages development of the Water Safety Group (WSG) which should facilitate a better understanding of factors that can adversely affect water quality.1
The WSP should include a detailed description of water systems, a risk assessment and management monitoring plan. Moreover, a review of governance procedures and training requirements should also be considered.
It is important to remember that European guidelines should be regarded as an example of good practice and can differ from national legislation. National legislation should always be adhered to where relevant; but where legislation exists, European guidelines can also be used to enhance investigations.
WATER SAFETY PLAN
Risk Areas that should be included in the WSP 1
A reasonably foreseeable risk of exposure to Legionella exists in buildings with:
- water systems incorporating an evaporative cooling tower and/or evaporative condenser;
- hot and cold-water distribution systems;
- natural thermal springs and their distribution systems
- spa pools (also known as hot tubs), whirlpool spas
- other systems including humidifiers, fountains and water features, and industrial water systems (e.g. air washers, wet scrubbers, vehicle washers, wastewater treatment plants/systems, misting devices and horticultural sprinkler systems);
- any other plant, systems or equipment containing water that is likely to be
- between 20°C and 45°C which may release a spray or aerosol during operation or demonstration, or when being maintained;
- any plant or system which uses water from a non-potable source (e.g. river water for evaporative cooling systems)
|
Temperature is one of the most important environmental factors influencing the growth of legionellae in water systems with growth occurring between 20°C and 45°C. While it is acknowledged that in many countries incoming cold-water temperatures below 20°C may not be achievable, the risk assessment should consider the potential risk of infection, which increases with higher temperatures. |
|
In hot water, if temperatures fall below 45°C, Legionella will grow. Although above 40°C many other bacteria which support the growth of legionella start to die, Legionella can still grow relatively quickly inside amoebae. How does temperature affect the growth of Legionella?
|
Do all water systems require a Water Safety Plan ?
Not all systems will require elaborate risk assessments and control measures. For smaller low-risk systems, the risk assessment may conclude that there is no reasonably foreseeable risk, or that the risks are insignificant and are being managed properly. No further action may be required at this stage, but existing controls must be maintained and monitored.
Who is responsible?
The responsibility for ensuring that water systems are managed to reduce the risk of infection falls upon:
- the building owner/employer - where there are risks from their business to their employees, visitors or others;
- a self-employed person - where there is a risk from their business to themselves or to others;
- the person who is in control of premises or systems - where there is a risk present from systems in the building;
- the person who is in control of premises used by visitors and the like for overnight accommodation (e.g. hotels, holiday apartments and campsites).1
Legionella Training - Who is Responsible?
Risk Assessment
The risk assessment is a critical component of a Water Safety Plan and should be regularly reviewed and updated. Checks should be made to ensure it includes consideration of:
- the identification of all the water systems, associated equipment and components
- the temperature of incoming water through all parts of the system
- the potential for aerosol generation;
- an up-to-date and valid schematic diagram;
- an assessment of the vulnerability of persons likely to be exposed;
- identification of areas which may not be used consistently (e.g. seasonal occupation or use in hotels rooms, sports pavilions and changing rooms or where water storage vessels have no or low turnover);
- assessment of each system for points where contamination could enter/occur, including during maintenance;
- assessment of factors which could promote the growth and dissemination of legionellae and other waterborne hazards;
- assessment of the effectiveness of the current control measures and the monitoring programme put in place to verify ongoing control, including: the results of on-site monitoring such as biocide levels, pH, temperature, turbidity, dissolved solids and dip slides (for cooling towers) together with the results of laboratory-determined microbiological and chemical parameters
- recommendations for improvement where needed,
- whether remedial actions have been taken as recommended in the risk assessment,
- appropriate and timely actions taken follow an adverse monitoring result;
- a review of governance procedures and the chains of communication are in place and up to date, including the management structure, the responsibilities and accountabilities of the individuals concerned, their training requirements and measurement of competence.1
|
Review of risk assessment and control measures – monitoring and routine inspection
If precautions are to remain effective, the condition of the system and performance of the control measures will need to be monitored. This should be the responsibility of the responsible person or, where required, a competent external contractor or an independent third party and should involve a process for:
- checking the performance of the system and its component parts;
- inspecting the accessible parts of the system for damage and signs of contamination, scale and corrosion;
- reviewing monitoring results to ensure that the treatment regime continues to control the system to the required standard. The frequency and extent of routine monitoring will depend on the operating characteristics of the system, but some should be carried out at least daily –e.g. checking that there is sufficient biocide available and that usage is within normal limits;
- testing of water quality, which is an essential part of the verification of the treatment regime, especially in cooling towers and spa pools. The type of tests required will depend on the nature and usage of the system;
- the routine monitoring of background bacterial counts (total viable count (TVC)) in evaporative cooling towers and spa pools.
- periodic sampling and testing for the presence of Legionella based on the risk assessment. This may also be appropriate as an indication that the control measures are effective.1
Microbiological monitoring
It is important to understand a sample taken from a water system is only a small proportion of the total system volume and that a negative Legionella result does not necessarily mean the entire system is safe and under control. Microorganisms are not uniformly distributed throughout the water system all of the time, especially in areas of poor flow and stagnation or where controls are not effectively maintained. Generally, water samples should be taken for routine sampling as the results are comparable over time and are therefore useful for trend analysis. However, in investigations, or when following up adverse results, swab samples may be a useful addition.
Action Levels
The European Guidelines identifies action levels for the high-risk water systems1:
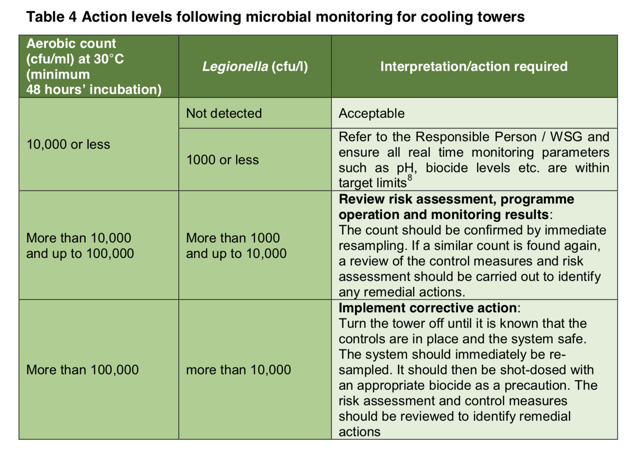
Action Levels following microbial monitoring for cooling towers (Table 4, page 73)
- 1000 CFU/L Action: Review Risk Assessment, programme operation and monitoring of results
- 10,000 CFU/L Action: Implement corrective action. 1
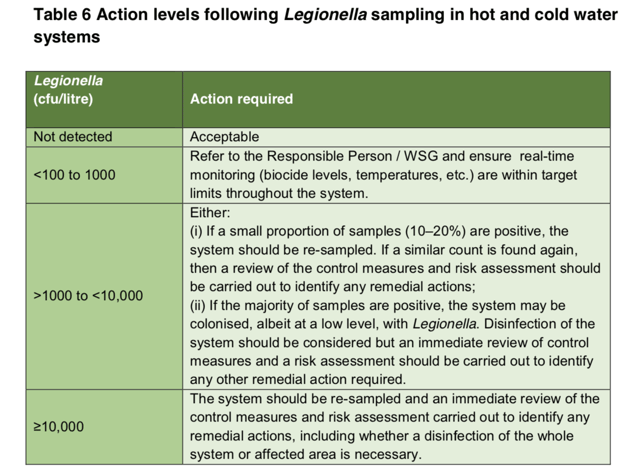
Action levels following Legionella sampling in hot and cold water systems (Table 6, page 96).
- 1000 CFU/L Action: Either resample, review controls measures, perform remedial actions OR Consider disinfection
- 10,000 CFU/L Action: Resample and immediately review control measures and carry out a risk assessment. 1
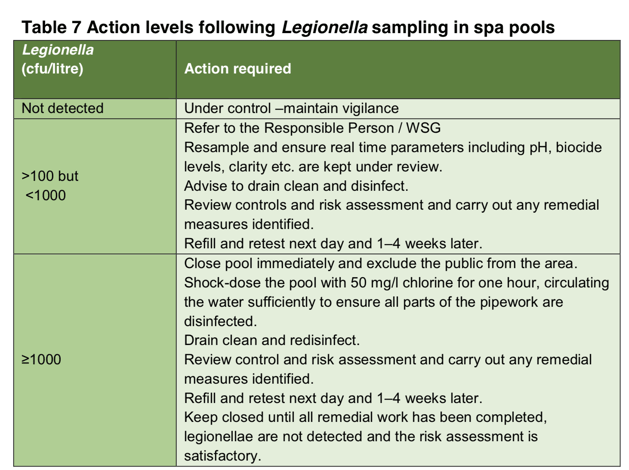
 Action levels following Legionella sampling in spa pools (Table 7, Page 100)
Action levels following Legionella sampling in spa pools (Table 7, Page 100)
- 10,000 CFU/L Action: Close pool immediately and exclude the public from the area. Shock-dose pool, drain, clean and disinfect.1
Testing for Legionella
Testing methods
The established method used worldwide for the detection and quantification of Legionella is the lab culture method known as ISO 11731. This method includes: sample collection, transport to the lab, growth (or culture) of the bacteria, analysis and production of a report. Legionella does not grow easily using culture methods and it takes 10-14 days to provide a result. Alternative methods for quicker detection of Legionella in water samples are also available on the market and may be used to facilitate continuous monitoring of water systems and ensure the safety of the public.
Alternative testing methods- rapid antigen testing
Regulations recommend periodic laboratory culture testing. However, compliance with regulations often is not enough to protect the public from risks associated with Legionella.
Alternative testing methods can provide an early warning of a potential problem and allow a fast response. If Legionella pneumophila is present in the system, it is inadvisable to wait two weeks to find out if people are being exposed to a potentially fatal infection. While carrying out laboratory culture tests might ensure compliance with the regulations, it can also be argued that not all reasonable measures have been taken to prevent an outbreak given the availability of the alternative testing methods. If the presence of Legionella in the system resulted in a fatality, it could be seen as negligence for not using an available, faster test.
Hydrosense Rapid Test
The Hydrosense Legionella antigen test utilizes lateral flow test technology, which is used in many medical tests for detecting Legionnaires’ disease in humans.
This innovative technology has been optimised to quickly detect cell surface Legionella antigen in all kinds of environmental water samples. The test is designed to be highly specific for Legionella pneumophila serogroup 1 - the species of Legionella which is responsible for 70 to 92% of laboratory-detected Legionellosis cases in the United States and Europe2.
The recovery rate of 80% in rapid-antigen testing is better than the lab culture method, which is typically 10-60%. 3 It also detects the viable but non-culturable (VBNC) and the motile phase of the Legionella pneumophila, which are the most virulent phases and cannot be detected by the lab culture method.
Rapid antigen testing is done on-site so there is no need to transport the samples to the lab. The results are then provided in 25 minutes.
The advantages of rapid ON-SITE testing include:
- better and more frequent monitoring;
- immediate knowledge, which supports fast action;
- time-saving and improved water quality.

Hydrosense reduces public and employee health risk by minimising the time taken to identify Legionella bacteria and capture results for ongoing verification and risk management requirements. In parallel with periodic lab testing, or as a stand-alone method, this simple test allows organisations to maintain vigilant control of water system quality. The test improves detection rates of Legionella bacteria and provides results, on-site and within minutes. Further result verification is provided by the Hydrosense smartphone reader and portal.
Find out more about Legionella testing methods available on the market.
Note: The above is a summary. Please refer to the latest version of the document when determining your water management plan.
References
- European Centre for Disease Control. (2017). Available at: http://bit.ly/2miMlJ9 [Accessed: 20 August 2018].
- Mercante, J. And Winchell, M. (2015). Available at: http://bit.ly/2kDSYpb [Accessed 6 May 2018].
- Polwart, N., Grant, R., Barnes, H., Holmes, E., Lindley, T. and Cooper, A. (n.d.). Available at: https://cdn2.hubspot.net/hubfs/3881041/IWC2008%20Paper%20%20.pdf [Accessed 19 Jul. 2018].
- Beauté, J. o. (2017). Available at: http://bit.ly/2mqYUCx [Accessed 28 Aug 2018].
- European Centre for Disease Prevention and Control (2015). Available at: http://bit.ly/2kUiiHk [Accessed 28 Aug 2018].
- Sakamoto R. (2015). Bull World Health Organ. 93(6):435-6. Available at: https://doi.org/10.2471/BLT.14.142299 [Accessed: 28 Aug 2018].
- Beauté J, Sandin S, Uldum SA, Rota MC, Brandsema P, Giesecke J, et al. (2016). Epidemiol Infect. 1-11. Available at: http://bit.ly/2miMuwb [Accessed: 28 Aug 2018].
- European Environment Agency (2012). Luxembourg: EEA; [online] Available at: http://bit.ly/2kpi8aO [Accessed: 28 Aug 2018].